Cells of the immune system
Introduction
- White blood cells or leucocytes serve as sentinels and defenders against infection.
- They move around the body via the lymphatic and blood circulatory systems.
- Leucocytes are classified by morphology- number of nuclei lobes and presence or absence of cytoplasmic granules.
- Leukocytes may be found as individual cells throughout the body, as accumulations within lymphoid organs (e.g., spleen, lymph nodes) and at sites of infection or inflammation.
- Knowledge of the role that each leukocyte plays is important in understanding immune function.
Formation of blood cells
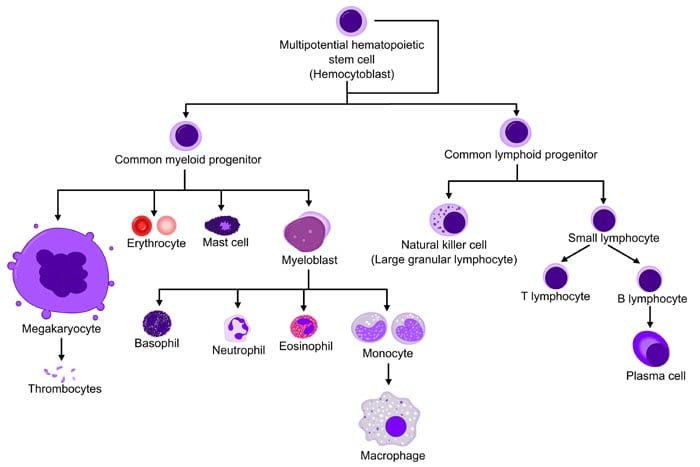
Flow chart of Haematopoiesis
All blood-borne cells originate in the bone marrow.
Pluripotent hematopoietic stem cells in the bone marrow give rise to two major lineages; a myeloid lineage and a lymphoid lineage.
Cells of the myeloid lineage differentiate further into platelets erythrocytes, eosinophils, basophils (and mast cells), neutrophils, monocytes/macrophages, and some dendritic cells.
Cells of the lymphoid lineage differentiate further into T and B lymphocytes, NK cells, and some dendritic cells.
Types of leucocytes
• White blood cells that have multilobed nuclei and contain conspicuous cytoplasmic granules are known as granulocytes.
• Others with a single, unlobed nucleus and cytoplasm that contains few or no granules are known as agranular leukocytes.
• A granular leukocytes derive from lymphoid or myeloid lineage precursors and account for approximately 35% to 38% of the leukocytes in circulation.
Cells of the innate immune system
• Myeloid Cells: First line of defense against invading organisms in non-specific innate immunity.
1. Neutrophils
2. Eosinophils
3. Basophils/Mast cells
4. Monocytes/Macrophages/Dendritic Cells
• Lymphoid Cells:
Neutrophils
• Comprises approximately 60% of the peripheral blood leukocytes, neutrophils are the most numerous leukocyte population.
• Neutrophils have multi-lobed nuclei (2-5) and cytoplasmic granules that stain with both acid and basic dyes.
• The neutrophil's main role is in inflammation. a) First to arrive at the inflammation site
b) Leave blood/endothelium into tissue (extravasation). • In the tissues, neutrophils are active phagocytes
• They destroy ingested microorganisms via oxygen-dependent or independent pathways.
• Deficiencies in pathways increase susceptibility to infections.
Eosinophils
• Eosinophils have bilobed nuclei and cytoplasmic granules that stain with the acid dye eosin
• Constitute 1%-3% of circulating leucocytes. • Involved in asthma.
• Eosinophils are motile, sometimes phagocytic, and are particularly active in parasitic infection.
Basophils
• Basophils have bilobed nuclei and cytoplasmic granules that stain with the basic dye methylene blue.
• Found in low numbers in the blood (<1%). Act like mast cells. • They are nonphagocytic
• Involved in allergic reactions (Type I hypersensitivity responses). a) Have high-affinity Fc receptors for IgE on their surface.
b) When an individual is exposed to an allergen, specific IgE is produced. This IgE binds to the surface of basophils.
c) Upon re-exposure to the allergen, the allergen binds to IgE on the surface of basophils resulting in degranulation.
d) Cross-linking of the IgE causes the basophils to release pharmacologically active mediators (histamine, prostaglandins, leukotrienes)
Mast cells
• Similar importance in allergic reactions as basophils, but only found in tissues.
• Contain granules with preformed mediators to be released after stimulation
a) histamine, prostaglandins
b) Leukotrienes
• Stimulation of mast cells occurs by the anaphylatoxins (complement proteins C3a and C5a) or by cross-linking of surface immunoglobulin (IgE).
Monocytes/Macrophages
• Circulate in the blood after leaving the bone marrow.
• Survive only a day or so before they enter the tissue to mature into
• Involved in phagocytosis and intracellular killing of microorganisms. a) Generation of toxic metabolites through respiratory burst.
b) Production of nitric oxide, hydrogen peroxide, superoxide anion.
Monocytes/Macrophages are antigen processing and presenting cells.
A) Degrative enzymes in lysosomal granules.
B) Chew ingested proteins.
C) Present to adaptive cells.
Macrophages
• When monocytes enter the tissues and become macrophages:
a) – Enlarge and increase the production of intracellular lysozymes
b) – Greater phagocytosis.
c) – Can live for years in tissue; highly motile.
• Activation of these cells occurs by phagocytosis of antigens, or in response to T cell-derived cytokines.
• Activated macrophages recognize and remove unwanted particulate matter including products of inflammation and invading organisms.
• After activation, these cells secrete cytokines, chemokines, lysozymes, and other factors to upregulate immune response. In chronic inflammation, macrophage scavengers can become “giant cells” or “foamy macrophages”.
Dendritic cells
• Specialized phagocytic cells found in most tissues.
• Arise both from the myeloid and lymphoid lineages.
• Abundant at interfaces between the external and internal environments (skin, the lining of the gastrointestinal tract), where they encounter invading pathogens.
• Actively motile; continuously sample surroundings by endocytic processes.
• Dendritic cells are very efficient at the activation of T cells. • More potent APCs than macrophages.
Natural Killer cells
• Also known as large granular lymphocytes (LG)
• Functionally cytotoxic representing an innate population that kills virally infected or tumor target cells.
• Killing is nonspecific - they do not need to recognize foreign antigens presented on the target cell.
v NK cells do not have a specific cell receptor. Target recognition occurs by a Killer
Inhibitory Receptor, KIR, which assess MHC I molecules on the target cell surface. MHC 1 molecule is lacking on infected and tumor targets.
• Kill targets by releasing perforin which damages target cell membranes. Can also induce apoptosis in the target cell.
• NK cells are different from NK T cells.
• NKT cells have some of the attributes of T cell and NK cell. Like T cells, NK1-T cells have T cell receptors (TCRs). Unlike most T cells, the TCRs of NK1-T cells interact with MHC-like molecules called CD1 rather than with class I or class II MHC molecules. Like NK cells, they have variable levels of CD16 and other receptors typical of NK cells, and they can kill cells.
Cells of the adaptive immune system
• Adaptive immune responses are mediated by a specialized group of leukocytes, the lymphocytes, which include T and B lymphocytes (T cells and B cells) that specifically recognize foreign material or antigens.
• All lymphocytes are derived from bone marrow stem cells, but T cells then develop in the thymus, while B cells develop in the bone marrow (in adult mammals).
B Lymphocytes
• Develop from stem cells in the bone marrow.
a) Produce antibodies with specificity for antigens and display them on their surfaces to function as BCRs.
b) Integral in humoral immunity
c) Plasma cells = terminally differentiated B cells that secrete immunoglobulins.
d) Memory cells- secondary immune response is swifter and stronger.
• Upon activation, a B cell can switch to produce a different class of antibody, with the same antigen specificity.
• Activation into antibody-secreting cells is antigen-dependent.
T-Lymphocytes
• T lymphocytes develop in the thymus.
a) Regulate immune responses.
b) Integral in cell-mediated immunity.
c) Critical in B cell-antibody production.
• Mature T cells display either CD4 or CD8.
a) Cells with a CD4 marker are called helper T cells (Th cells).
b) CD8 marker positive cells are cytotoxic T cells (Tc cells).
• There are several different types of T cell, and they have a variety of functions :
a) Type 1 helper T cells or TH1 cells - interact with mononuclear phagocytes and helps them destroy intracellular pathogens•
b) Type 2 helper T cells or TH2 cells; interacts with B cells and helps them to divide, differentiate, and make antibody•
c) Cytotoxic T lymphocytes (CTLs or TC cells). responsible for the destruction of host cells that have become infected by viruses or other intracellular pathogens.
d) Regulatory T cells or Tregs, help to control the development of immune responses and limit reactions against self-tissues.
Conclusion
• The immune system has evolved to protect us from pathogens.
• Phagocytes and lymphocytes are key mediators of immunity. Phagocytes internalize pathogens and degrade them. Lymphocytes (B and T cells) have receptors that recognize specific molecular components of pathogens and have specialized functions. B cells make antibodies (effective against extracellular pathogens), cytotoxic T lymphocytes (CTLs) kill virally infected cells, and helper T cells coordinate the immune response by direct cell-cell interactions and the release of cytokines.
• The immune system may fail (immunopathology). This can be a result of immunodeficiency, hypersensitivity, or dysregulation leading to autoimmune diseases.
Thanks & Regards
Vikas Tiwari


👌👌
ReplyDeletegood
ReplyDelete