Insulin Tolerance Test
Introduction:-
An insulin tolerance test (ITT) is a medical diagnostic procedure during which insulin is injected into a patient's vein, after which blood glucose is measured at regular intervals.
Indication(s)
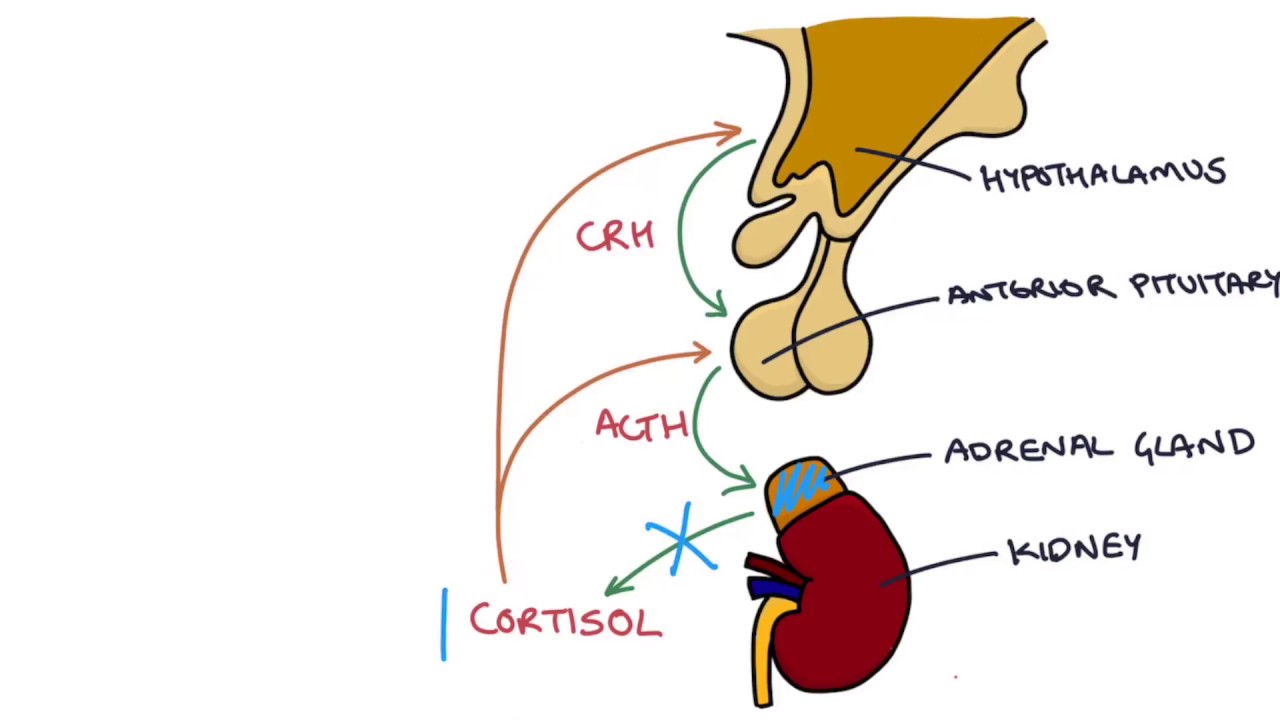
Investigation of the hypothalamic-pituitary axis (HPA) with regard to the release of growth
hormone (GH) and adrenocorticotropic hormone (ACTH). Typically used for the investigation
of suspected growth hormone deficiency. Sometimes used for the investigation of
glucocorticoid deficiency when other investigations (such as the synacthen stimulation test)
are not appropriate. If random GH and cortisol samples demonstrate clearly sufficient levels
there is no need to perform this test.
:max_bytes(150000):strip_icc()/how-do-i-know-if-i-have-insulin-resistance-2616646-v2-5c455306c9e77c0001db3ac7.png)
Background
The stress of insulin-induced hypoglycemia triggers the release of GH and ACTH from the
pituitary gland in normal subjects. GH response is measured directly. ACTH is typically
measured indirectly using cortisol but may be measured directly.
Precautions/Contraindications
This test is absolutely contraindicated in patients with epilepsy, cardiac rhythm disturbances,
ischaemic heart disease, previous cerebrovascular accidents, or any unexplained fits or
collapses.
A medical officer should be present from the administration of insulin until the blood sugar
the level has returned to greater than 3.0 mmol/L and is no longer dropping.
Patient Preparation
- Oestrogen containing medications such as hormone replacement therapy (HRT) or the oral contraceptive pill (OCP) must be stopped six weeks prior to this test. These medications can affect steroid hormone-binding globulin levels.
- If testing ACTH secretion, then glucocorticoids need to be omitted for an appropriate amount of time (discuss with requesting doctor) before the test to prevent interference with both the HPA axis and the cortisol assay.
- Patients should fast from midnight (with only water to drink) before the test.
- Patients should be asked to bring their medications with them to
- be documented for the test and
- be taken at the completion of the test.
- Patients should bring a meal containing carbohydrates (e.g. a sandwich) to end the fast at the completion of the test.
- Pre‐test workup includes an ECG, 9 am cortisol and free thyroxine level. These should all be performed and checked by the requesting doctor before proceeding with this test.
- The requesting doctor must make an evaluation of the insulin dose needed for the test. A guideline is provided below:
- Sensitive (e.g. panhypopituitarism): 0.1 U/kg single bolus
- Standard: 0.15 U/kg single bolus
- Known to have acromegaly: 0.3 U/kg single bolus
- Diabetic: 0.5 ‐1.0 U/hour insulin infusion with 0.15 U/kg single bolus once BSL is < 9 mmol/Liii
Equipment
Intravenous infusion and blood collecting equipment
- This test requires an IV cannula to Administer the insulin dose
- Take repeated blood samples
- Give emergency rescue dextrose if necessary
- Point of care glucometer
- Blood sample tubes
A) 10 x 4 mL Serum separator clot activator tubes (red top, yellow centre) for cortisol/growth hormone
B) 10 x 2 mL Sodium fluoride/potassium oxalate (grey top, white centre) tubes for glucose
C) 6 x 3.5 mL Potassium EDTA (purple top, black centre) tubes for ACTH
- Ice for ACTH samples
- Blood pressure and heart rate measuring equipment
- Thermometer
- Weighing scales, tape measure, stadiometer (height measurement)
- Short-acting insulin for intravenous administration
Use human neutral insulin ‐ “Actrapid”
- vials of 50 mL of 50% Dextrose
- 1 Litre 0.9% (normal) saline
- Meal to feed patient following test (brought in by patient)
- 75 g glucose drink

Procedure
This test must be performed by a doctor or nurse with endocrine training. This test may be performed at any time. However given the need to fast 8 hours, it is generally performed in the morning to minimise inconvenience to the patient. Read through the entire test protocol before beginning. Ensure you have all equipment ready. Explain and consent the patient for the procedure. Record general observations including; blood pressure, pulse rate, temperature, weight, height and waist circumference on the flow‐sheet.
Insert an intravenous cannula in the antecubital fossa and commence a slow infusion of 0.9% (normal) saline (50mL/hour) to maintain venous patency. Once the cannula has been inserted and the patient is resting, collect the first set of blood samples for glucose and growth hormone/cortisol/ACTH (as per the request). Record the time in the ‐15 minutes section of the flow‐sheet.
Wait 15 minutes after inserting the cannula (to eliminate a temporary rise in cortisol associated with the needle stick), then collect the second set of baseline blood. Record the time in the 0 minutes section of the flow‐sheet.
Immediately after the second set of baseline blood samples have been collected administer the intravenous insulin at the dose prescribed by the requesting clinician. Use the point of care glucometer to perform a blood sugar level (BSL) every 5 minutes after insulin administration. Fill the results in on the corresponding time section of the flow‐sheet provided. Note any symptoms of hypoglycaemia in the comments section. At times 30 minutes, 45 minutes, 60 minutes, 90 minutes and 120 minutes take a blood sample for glucose and growth hormone/cortisol/ACTH.
Adequate hypoglycaemia is defined as a whole blood glucose of less than or equal to 2.2 mmol/L accompanied by symptoms of hypoglycaemia (e.g. sweating, tachycardia and drowsiness). This usually occurs 30 ‐ 45 minutes after iv insulin is administered, but can happen much sooner.
If adequate hypoglycaemia is not achieved by 45 minutes, give a second bolus dose of intravenous insulin, 50% higher than the initial dose. At this point, the documentation of the test should continue on a new flow‐sheet noting the time of the second dose of insulin in the 0-minute section.
If adequate hypoglycaemia is still not achieved 30 minutes after the second dose, give a third bolus dose of intravenous insulin that is twice the initial dose. At this point, the documentation of the test should continue on another new flow‐sheet noting the time of the third dose of insulin in the 0-minute section.
If adequate hypoglycaemia is still not achieved 30 minutes after the third bolus of insulin then contact the requesting clinician for advice.
The patient should be observed closely following the achievement of adequate hypoglycaemia (< 2.2 mmol/L).
In most cases, a gradual rise in BSL occurs spontaneously due to the secretion of counter-regulatory hormones.
Occasionally, the BSL may continue to fall. If the BSL drops to 1.6 mmol/L or less, 25 mL of 50% intravenous Dextrose must be administered to avert the risk of severe hypoglycaemia which may cause loss of consciousness or seizure. In the rare event that a sustained increase in blood glucose > 2.2 mmol/L is not achieved then a second 25 mL dose of intravenous 50% dextrose should be administered.
At the conclusion of the insulin tolerance test (120 minutes after insulin administration), blood glucose levels will usually have recovered to > 3.5 mmol/L. Ask the patient to eat the meal they brought in with them. If the blood glucose level at 120 minutes is < 3.5 mmol/L, give a 75g glucose drink in addition to the patient’s meal.
Thanks & Regards
Vikas Tiwari


Comments
Post a Comment